Improving the sleep rate of
preterm infants
The project — aptly named “Sleep Well Baby” — was a great success, winning the National Award for Best Innovation and leaving the door open for future work in this important area.

05-2019
Author: James Rowbotham (Meet Our Team)
In the field of healthcare, Dutch Hacking Health is the largest hackathon event in the Netherlands. It brings healthcare professionals, researchers, patients, developers and data scientists together to try and solve some of the most pressing healthcare related issues the industry currently faces.
For the past three years, Finaps has sent a team of engineers to the University Medical Centre in Utrecht (UMCU) to help come up with a technology-based solution to one of the issues that medical professionals at the hospital have highlighted.
Last year, Finaps brought home the Best Data Driven award for a patient data visualisation tool — “Ur Smart Status” — which aimed to improve the way medical professionals interpret patient data. Since then, Ur Smart Status has entered into its second phase of development backed by Finaps and the Applied Data Analytics in Medicine’ (ADAM) project at the UMCU.
This year, working alongside medical specialists from the Neonatal Intensive Care Unit (NICU) and data scientists from the UMCU, the Finaps team was tasked with the challenge of creating a predictive algorithm that could help determine whether an infant is asleep or awake.
The project — aptly named “Sleep Well Baby” — was a great success, winning the National Award for Best Innovation and leaving the door open for future work in this important area.
Project Background
Why do Babies Need to Sleep so Much?
We are only just starting to wake up to the critical importance of sleep for an infant’s mental and physical development.
Although all developmental stages of the foetus are crucial, the last trimester seems to be the most important for determining later cognitive and behavioural outcome. It appears that in the last fourteen weeks of pregnancy the connections in the brain are reorganised and the first blue print for the final outline of the brain is completed.
The Term/Preterm Distinction
For infants born before term age is reached — before 37 weeks of gestation — these brain development stages happen outside of the womb. These infants are known as “preterm”.
Preterm infants receive advanced care at the NICU because of their severe vulnerability. In many cases they are unable to breath without assistance, unable to regulate their own body temperature, and are at a higher risk of infection than “term” infants.
Accordingly, preterm infants are at a high risk of incurring brain injury and abnormal neurodevelopmental outcome and must be intensively monitored to be kept alive.

Optimising Brain Development
Finding ways to optimise brain development is one of the most important goals of Neonatology.
Unfortunately, one of the most important factors in brain development is yet to be fully incorporated into the infant care plan: sleep optimisation.
Being data-driven is
a spectrum: it is not binary
– you can always become
more data-driven
The Problem
Animal research highlights the importance of sleep for neonatal brain development. Suggesting that for preterm infants, who are at the highest risk of adverse neurodevelopmental outcome, sleep is of even higher importance.
Despite this knowledge, infants that are admitted to the NICU do not sleep enough.
Highly specialised hospital wards like the NICU are crammed full of noisy equipment, bright lights and busy medical professionals. All of which are vital for an infant’s life, but can easily disrupt their natural sleep rhythm. In addition to this, infants are often woken up when it’s time for care or when a medical procedure is required.
Finding ways to minimise sleep disturbance is therefore of critical importance.
Medical staff often neglect an infant’s natural sleep cycle, basing judgement of when to perform elective procedures primarily on time of day or routine.
The Golden Standard
The current best practise is for a trained medical professional to monitor an infant as they sleep. During monitoring, visual sleep classifications (VSC) — behavioural signs associated with sleep state — are used to determine whether an infant is awake or asleep, and in which sleep state they are in.
Unfortunately, this highly personalised healthcare comes at a high cost, both in terms of training time and manpower.
The Solution
An alternative to VSC, involves routine monitoring data, such as heart and respiration rate. By coupling this data to sleeping scores, a predictive algorithm could be developed, which would automate the process of detecting an infant’s sleep state.
Once sleep state is ascertained, a medical specialist could schedule medical procedures and feeding times around an infant’s natural sleep rhythm.
Project Objective
To maximise the sleep time of preterm infants using a predictive algorithm that can determine whether an infant is asleep or awake.
Literature Review
A systematic review of the literature pointed us towards the physical parameters that are the most reliable indicators of sleep state and that are currently being measured by the NICU.
These include:
— Heart rate
— Diastolic blood pressure
— Systolic blood pressure
— Mean blood pressure
— Respiration rate
— Saturation
Data Collection
The VSC data was collected through observation. Three trained medical specialists scored the sleep state of 20 subjects every minute for three hours. This resulted in 3600 labelled observations of sleep state.
Additionally, all of the above-mentioned physical parameters were recorded once every 2.5 seconds.
Feature Engineering
For each parameter we constructed the mean, minimum, maximum, median and standard deviation at 1, 2 and 5 minute intervals. In addition to this, metadata including gender and age were recorded.
Model
We attempted to model a simple yes/no (0/1) decision process — Is the infant asleep or awake?
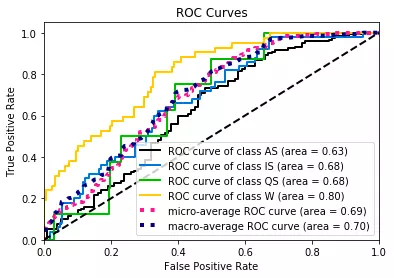
Multiple models were tested for best fit, including logistic regression, random forest and gradient boosting. The latter was found to be the best performing model — Recording a Best Area Under Curve of 0.80 (green in the chart graph below)
Data Visualisation
To visualise the working algorithm, we built a dashboard using React.js. The dashboard features several key parameters visualised using Plotly, and a corresponding pie chart that displays the probability that the infant is in a sleep or awake state. Please note: the data fetching was sped up for a better demonstration of the algorithm in action.
What’s Next?
The purpose of Dutch Hacking Health is to prototype innovative solutions to some of the real-world issues that the Dutch healthcare industry currently faces.
It’s important to note, that given the time and resource constraints that come with hackathons, the result of our project is by no means the finished product. A second iteration might attempt to model the sleep state with greater accuracy and would likely explore the different types of sleep an infant experiences.
Nonetheless, this project represents the start of an exciting new avenue of innovation that, not only has practical utility in the everyday functioning of a hospital, but is also a great example of how the technology and healthcare industries can come together to improve healthcare.
Finaps would like to thank Dr. Jeroen Dudink, Eline de Groot, Marit Knoop, Jing Qin, Charlotte Teunis, Dr. Daniel Vrijbrief, Dr. Agnes van den Hoogen and the Head of the Neonatal Department Prof. Dr. Manon Benders from the UMC for all their hard work in conducting the background research, collecting data, and for their enthusiasm and deep understanding of the problem that we are aiming to solve. We would also like to thank O’Jay Medina and Sebastiaan Broekema from the UMC Applied Data Analytics Department who, together with Finaps, provided the technical knowhow to bring this idea into fruition.
For more information about this topic you can visit this link: https://onlinedocu.nl/slaap/